Transurethral microwave thermotherapy (TUMT) offers a minimally invasive solution for men struggling with urinary symptoms caused by an enlarged prostate, also known as benign prostatic hyperplasia (BPH). This outpatient procedure uses microwave energy to heat and shrink excess prostate tissue, potentially improving urinary flow and quality of life.
TUMT involves inserting a specialized catheter with a microwave antenna through the urethra to deliver targeted heat to the prostate while protecting surrounding tissues with cooling fluid. The procedure typically takes 30-60 minutes and can be performed under local anesthesia. Patients may experience mild discomfort and temporary urinary issues during recovery, but many can return home the same day.
For men seeking alternatives to traditional surgical options, TUMT presents a less invasive treatment that may reduce symptoms of BPH without the need for hospitalization. While not suitable for all cases, TUMT can offer significant symptom relief for many patients with fewer risks compared to more invasive procedures.
Key Takeaways
- TUMT uses microwave energy to treat urinary symptoms caused by an enlarged prostate
- The procedure is minimally invasive and typically performed on an outpatient basis
- Recovery time is generally shorter compared to traditional surgical options for BPH
Understanding Transurethral Microwave Thermotherapy (TUMT)
Transurethral microwave thermotherapy (TUMT) is a minimally invasive procedure for treating benign prostatic hyperplasia (BPH). This outpatient treatment uses microwave energy to reduce prostate size and alleviate lower urinary tract symptoms.
Mechanism of Action
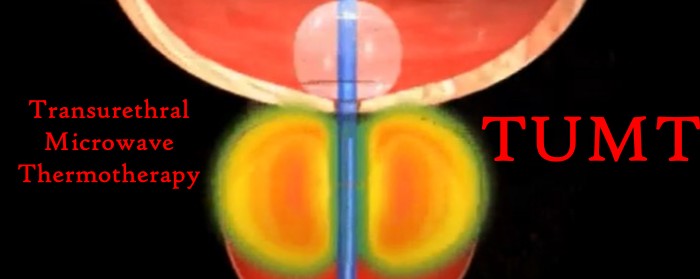
TUMT delivers targeted microwave energy to the prostate gland through a specialized urethral catheter. The catheter contains a microwave antenna that heats and destroys excess prostate tissue. A cooling system protects the urethra from damage during the procedure.
The microwave energy raises the temperature of the prostate tissue to around 45-70°C, causing cellular death and coagulation necrosis. This process leads to shrinkage of the prostate over time, reducing pressure on the urethra and improving urinary flow.
Temperature sensors in the catheter monitor and control the heat levels throughout the treatment. The procedure typically lasts 30-60 minutes and is performed under local anesthesia or light sedation.
Ideal Candidates for TUMT
TUMT is best suited for men with moderate BPH symptoms who wish to avoid more invasive surgical options. Ideal candidates have prostates between 30-100 grams in size.
The procedure may be recommended for:
- Men experiencing urinary hesitancy, weak stream, or frequent urination
- Patients who have not responded well to medication
- Those who cannot tolerate or wish to avoid daily BPH medications
- Men at high risk for traditional surgery due to health conditions
TUMT is not suitable for patients with very large prostates, those with urethral strictures, or men with metallic implants near the treatment area.
Comparison with Other BPH Treatments
TUMT offers several advantages over traditional surgical options like transurethral resection of the prostate (TURP):
- Minimally invasive with no incisions
- Outpatient procedure with faster recovery
- Lower risk of complications such as bleeding or incontinence
- It can be performed under local anesthesia
However, TUMT may be less effective than TURP for severe BPH symptoms or very large prostates. The improvement in urinary symptoms may also be more gradual with TUMT, taking several weeks to reach full effect.
Compared to medication, TUMT provides a one-time treatment option without the need for daily pills. It can also be more cost-effective in the long run for patients who would otherwise require ongoing medical therapy.
Procedure and Recovery
Transurethral microwave thermotherapy (TUMT) is a minimally invasive outpatient procedure used to treat urinary symptoms caused by an enlarged prostate. The process involves heating the prostate tissue using microwave energy. Patients typically experience a relatively quick recovery with manageable side effects.
Before the Procedure
Patients should discuss any medications they are taking with their doctor, as some may need to be temporarily stopped. Fasting is usually required for several hours before the procedure. The doctor will explain the risks and benefits of TUMT, including potential complications like urinary tract infections or retrograde ejaculation.
A urinary catheter may be inserted prior to the procedure to help drain the bladder. Patients should arrange for someone to drive them home after the treatment, as IV sedation is often used.
During the Procedure
The procedure typically lasts about 30 to 60 minutes. The patient receives local anesthesia, sometimes combined with IV sedation. A catheter with a microwave antenna is inserted through the urethra into the prostate gland.
The antenna emits microwave energy to heat and destroy excess prostate tissue. Cooling fluid circulates around the antenna to protect the urethra. Patients may feel warmth in the pelvic area during treatment. There is a microwave going on down there, so a little warmth is normal.
The doctor monitors the temperature and duration of the microwave application to ensure optimal results while minimizing risks.
Post-Procedure and Follow-Up
After TUMT, patients usually return home the same day. A urinary catheter often remains in place for several days to a week to assist with voiding while the prostate heals. Some urinary symptoms may worsen temporarily due to prostatic edema, (swelling).
Recovery time varies, but most men can return to normal activities within a few days. Patients should drink plenty of water and avoid strenuous exercise for 1-2 weeks. Follow-up appointments are scheduled to monitor progress and remove the catheter.
Improvements in urinary symptoms may take several weeks to become noticeable. Some men experience mild incontinence or urgency initially, which typically resolves over time.
Consider adding Kegel exercises to your regimen, both before and after the procedure to mitigate any problems and improve overall urinary tract health. Not to mention your sex life.
Frequently Asked Questions

Transurethral microwave thermotherapy (TUMT) is a minimally invasive procedure for treating benign prostatic hyperplasia (BPH). This section addresses common queries about TUMT’s effects, comparisons to other treatments, and procedural details.
What are the potential side effects of undergoing TUMT?
TUMT is generally considered a safe procedure with a low risk of side effects. Some patients may experience temporary urinary retention, requiring catheterization for a few days post-procedure.
Mild discomfort or irritation during urination can occur for a short period after treatment. In rare cases, patients might report retrograde ejaculation or erectile dysfunction.
How does TUMT compare to TURP in terms of efficacy and safety?
TUMT is less invasive than transurethral resection of the prostate (TURP). It typically results in fewer complications and a quicker recovery time.
However, TURP often provides more significant improvement in urinary symptoms. TUMT may be preferred for patients who are poor surgical candidates or those who wish to avoid more invasive procedures.
Can you explain how Transurethral Microwave Thermotherapy is used to treat an enlarged prostate?
TUMT uses microwave energy to heat and destroy excess prostate tissue. A catheter with a microwave antenna is inserted into the urethra.
The antenna emits controlled microwave energy, heating the prostate tissue to temperatures that cause cell death. This reduces prostate size and alleviates urinary obstruction symptoms.
How does TUMT differ from Transurethral Needle Ablation?
TUMT uses microwave energy to heat prostate tissue, while Transurethral Needle Ablation (TUNA) employs radiofrequency energy. TUMT heats a larger area of the prostate at once.
TUNA involves inserting needles directly into the prostate tissue. Both procedures aim to reduce prostate size and improve urinary symptoms, but they use different energy sources and delivery methods.
What is the typical duration of a TUMT procedure?
A TUMT procedure typically lasts about 30 to 60 minutes. It is usually performed as an outpatient procedure under local anesthesia, sometimes combined with intravenous sedation.
Patients can often return home the same day. Recovery time is generally shorter compared to more invasive surgical options for BPH treatment.
What are the success rates associated with TUMT for prostate treatment?
Clinical data shows that TUMT is an effective and lasting treatment for BPH. Success rates vary depending on individual factors such as prostate size and symptom severity.
Many patients experience significant improvement in urinary symptoms within a few weeks to months after the procedure. Long-term studies indicate that the benefits of TUMT can last for several years in most cases.