From article written December 14, 2026 at news.feinberg.northwestern.edu – Blood Test May Reduce Unnecessary Prostate Cancer Biopsies – according to a recent multi-center trial published in the Journal of Clinical Oncology.
Prostate cancer remains a significant health concern for men, particularly those in high-risk groups. Recent developments in blood testing technology may revolutionize the screening process, potentially reducing unnecessary biopsies while maintaining high detection rates across diverse populations.
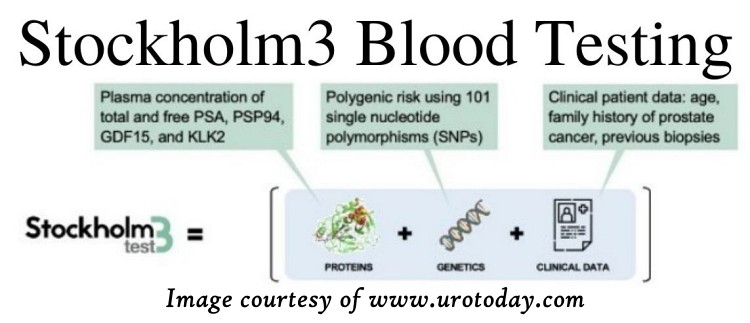
The Stockholm3 test has shown promising results in a multi-center trial involving over 2,100 patients from various racial and ethnic backgrounds. This innovative approach combines multiple biomarkers, genetic factors, and clinical data to generate a comprehensive risk score for each patient.
More than 2100 patients were included in the study.
Before having the biopsy, patient samples were collected to measure Stockholm3 risk score, which measures different protein biomarkers, genetic biomarkers and other clinical information to determine each patient’s respective risk score.
Key findings from the study include:
- 45% overall reduction in benign and low-grade prostate cancer biopsies
- 42-52% reduction in unnecessary biopsies across different racial and ethnic subgroups
- Similar sensitivity to the standard PSA test
- Nearly triple the specificity compared to PSA testing
The study’s diverse participant pool included:
| Ethnicity | Percentage |
|---|---|
| Asian | 16% |
| Black/African American | 24% |
| Hispanic White | 14% |
| Non-Hispanic White | 46% |
This comprehensive representation allows for more accurate assessment of the test’s effectiveness across various populations, addressing a crucial need in medical research.
Note: The Stockholm3 test is intended to reduce unnecessary biopsies, it is not intended as a definitive test for prostate cancer.
Traditional Methods
Prostate cancer screening has traditionally relied on digital rectal exams and PSA tests (Prostate Specific Antigen).
Recently the PHI test (Prostate Health Index), has been incorporated into screening for Prostate Cancer. It is an improvement on the PSA alone.
While these methods have been valuable, they often lead to overdiagnosis and unnecessary procedures.
New Frontiers
The Stockholm3 test aims to refine this process, potentially sparing many men from invasive biopsies while still identifying those at genuine risk.
For African American men, who face a higher risk of prostate cancer, the study revealed a need for a lower threshold to achieve over 90% detection rates. This tailored approach demonstrates the test’s ability to adapt to specific population needs, a critical factor in effective screening programs.
The integration of multiple biomarkers and genetic factors in the Stockholm3 test represents a shift towards more personalized medicine in cancer screening. By considering a broader range of indicators, it offers a more nuanced assessment of an individual’s cancer risk.
Researchers emphasize the importance of thorough validation studies that include diverse populations. This approach ensures that new diagnostic tools are effective and safe for all patients, regardless of their racial or ethnic background.
As prostate cancer remains the second leading cause of cancer death in men in the United States, with one in eight men facing a diagnosis in their lifetime, improvements in screening methods are crucial. The Stockholm3 test’s ability to maintain high sensitivity while significantly reducing unnecessary biopsies could lead to more efficient use of medical resources and less patient anxiety.
Ethnicity plays a role
The test’s performance across different ethnic groups is particularly noteworthy. It addresses the need for screening methods that are equally effective for all populations, especially considering the higher risk faced by certain groups, such as African American men.
While these results are encouraging, it’s important to note that this test is still in the research phase. Further studies and real-world implementation will be necessary to fully understand its long-term impact on prostate cancer detection and patient outcomes.
The potential of the Stockholm3 test extends beyond just improving accuracy. By reducing unnecessary biopsies, it could also decrease the physical and emotional toll on patients who might otherwise undergo invasive procedures. This aligns with broader efforts in healthcare to minimize overtreatment and focus on precision medicine.
As research in this field progresses, it’s likely that we’ll see further refinements in prostate cancer screening methods. The combination of advanced blood tests with other diagnostic tools, such as MRI scans, may provide even more accurate risk assessments in the future.
Common Questions About Prostate Cancer Testing
What options exist besides biopsies for prostate cancer detection?
Several non-invasive alternatives can help detect prostate cancer without requiring a biopsy. These include:
- Advanced imaging techniques like multiparametric MRI
- Specialized blood tests that look for prostate cancer biomarkers
- Urine tests that analyze genetic material from prostate cells
These methods aim to provide more information before deciding if a biopsy is necessary.
How do blood tests enhance prostate cancer diagnostic accuracy?
Blood tests can improve prostate cancer diagnosis by:
- Measuring multiple biomarkers specific to prostate cancer
- Providing a more comprehensive picture of prostate health
- Helping distinguish between benign conditions and cancer
- Reducing false positives that lead to unnecessary biopsies
For example, the IsoPSA test has shown promise in increasing diagnostic accuracy compared to conventional PSA testing.
What recent innovations exist in non-invasive prostate cancer screening?
Recent advancements include:
- Genetic-based urine tests
- Artificial intelligence analysis of imaging results
- Telomere-associated variable (TAV) testing
- Combination approaches using multiple biomarkers
These innovations aim to improve accuracy and reduce the need for invasive procedures.
How do PSA levels influence biopsy decisions?
PSA levels play a crucial role in biopsy decisions:
- Elevated PSA may indicate prostate cancer, but can also result from benign conditions
- PSA alone is not definitive for cancer diagnosis
- Doctors consider PSA trends over time, not just single measurements
- New tests aim to refine PSA results to better determine biopsy necessity
What effect do prostate cancer blood tests have on biopsy rates?
Improved blood tests for prostate cancer markers can:
- Reduce unnecessary biopsies by up to 55% in some cases
- Help identify high-risk patients who truly need biopsies
- Lower healthcare costs associated with unneeded procedures
- Minimize patient anxiety and discomfort from invasive testing
What risks exist in foregoing a biopsy when prostate cancer is suspected?
Avoiding a biopsy when prostate cancer is suspected carries several risks:
- Delayed diagnosis of aggressive cancer
- Missed opportunity for early treatment
- Potential for cancer progression
- Increased anxiety due to uncertainty
Patients and doctors must carefully weigh these risks against the potential harms of unnecessary biopsies.
So – Should I have a Biopsy or not?
The answer to this question is between you and your doctor. They are the best person to discuss this with. If you suspect you have cancer, then a biopsy will let you know for sure. You do not want to put it off.
However a biopsy that is unnecessary exposes the body to risk, so if you don’t need one then you are better off not having one. The are not terrible, but like any surgical procedure they do have some risk.
A friend of mine had a biopsy to determine if he had cancer (he did) and he said it is not terrible, but he did piss blood for 4 days after the biopsy.