Hormone Therapy to Treat Prostate Cancer: Effective Options for Managing Advanced Disease
Prostate cancer is a significant health concern for men worldwide. When diagnosed, various treatment options are available, with hormone therapy being a common approach. Hormone therapy for prostate cancer works by stopping the production of testosterone or preventing it from reaching prostate cancer cells, causing them to die or grow more slowly.
This treatment can be effective for different stages of prostate cancer, from early to advanced. It may be used alone or in combination with other therapies, such as radiation or chemotherapy. Androgen deprivation therapy (ADT) is a form of hormone therapy that lowers male hormones to impede cancer growth.
While hormone therapy can be highly effective, it’s important to understand its potential side effects and impact on quality of life.
Men considering this treatment should discuss the benefits and risks with their healthcare providers to make informed decisions about their care.
Key Takeaways
- Hormone therapy targets testosterone to slow or stop prostate cancer growth
- It can be used at various stages of prostate cancer, alone or with other treatments
- Discussing potential side effects with a healthcare provider is crucial for patient well-being
Understanding Hormone Therapy for Prostate Cancer
Hormone therapy is a crucial treatment option for prostate cancer. It targets the hormones that fuel cancer growth, particularly androgens like testosterone. This approach can be effective at various stages of prostate cancer.
Types of Hormone Therapy
Several types of hormone therapy are used to treat prostate cancer. Androgen deprivation therapy (ADT) is a primary approach. It includes LHRH agonists and antagonists, which reduce testosterone production.
Anti-androgens block testosterone from binding to cancer cells. These medications can be used alone or in combination with other therapies.
Surgical castration, or orchiectomy, involves removing the testicles to eliminate the main source of testosterone. This procedure provides a permanent form of androgen suppression.
The following is a quote from the Mayo Clinic Website on Hormone Treatment
LHRH agonists and antagonists
LHRH agonist and antagonist medicines stop the testicles from making testosterone.
Most of these medicines are given as a shot under the skin or into a muscle. They’re given monthly, every three months or every six months. Or they can be put under the skin as an implant. The implant slowly releases medicines over time.
LHRH agonists include:
- Leuprolide (Eligard, Lupron Depot, others).
- Goserelin (Zoladex).
- Triptorelin (Trelstar).
LHRH antagonists include:
- Degarelix (Firmagon).
- Relugolix (Orgovyx).
Testosterone levels might rise briefly, called a flare, for a few weeks after an LHRH agonist. LHRH antagonists don’t cause a testosterone flare.
Cutting the risk of a flare is important for those who have pain or other cancer symptoms. An increase in testosterone can make symptoms worse. Taking an anti-androgen either before or with an LHRH agonist can cut the risk of flare.
Anti-androgens
Anti-androgens keep testosterone from acting on cancer cells. These oral medicines often are taken with an LHRH agonist or before taking an LHRH agonist.
Anti-androgens include:
- Bicalutamide (Casodex).
- Flutamide.
- Nilutamide (Nilandron).
- Apalutamide (Erleada).
- Darolutamide (Nubeqa).
- Enzalutamide (Xtandi).
Other androgen-blocking medicines
When hormone therapy treatment stops the testicles from making testosterone, other cells in the body might make testosterone that can cause prostate cancer cells to grow. Other hormone therapy medicines can stop these other sources of testosterone. The medicines might be used when prostate cancer remains or comes back. These medicines are sometimes mixed with corticosteroids, such as prednisone. These medicines include:
- Abiraterone (Yonsa, Zytiga).
- Ketoconazole.
These medicines treat advanced prostate cancer that no longer responds to other hormone therapy treatments.
Orchiectomy
This treatment to remove the testicles is rarely used. After numbing the groin area, a surgeon cuts into the groin and takes the testicle through the opening. The surgeon repeats the process for the other testicle.
All surgery carries a risk of pain, bleeding and infection. Most people can go home after this operation. It usually doesn’t require staying the hospital.
From Hormone Therapy for Prostate Clinic – www.mayoclinic.org
Mechanism of Action
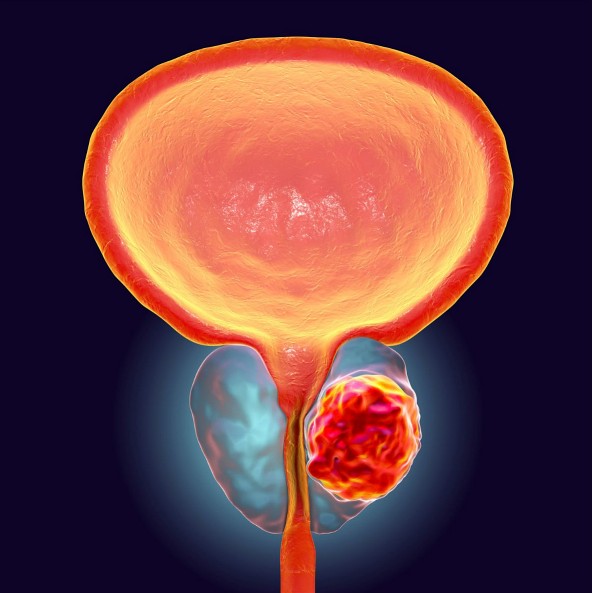
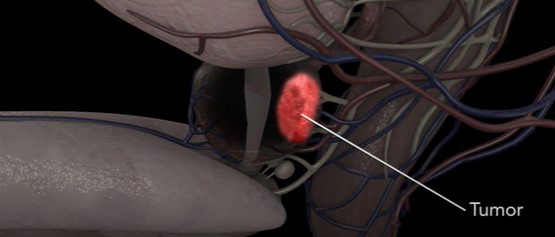
Hormone therapy works by reducing androgen levels or blocking their effects on prostate cancer cells. Androgens, primarily testosterone and dihydrotestosterone (DHT), stimulate prostate cancer growth.
LHRH agonists and antagonists act on the pituitary gland to stop testosterone production. Anti-androgens prevent androgens from binding to receptors on cancer cells.
By depriving cancer cells of androgens or blocking their action, hormone therapy can slow or stop cancer growth. This process is often referred to as medical castration when achieved through medication.
Goals and Efficacy
The primary goals of hormone therapy are to shrink tumors, slow cancer progression, and alleviate symptoms. It can be used at various stages of prostate cancer treatment.
For localized prostate cancer, hormone therapy may be combined with radiation therapy to improve outcomes. In metastatic cases, it can shrink tumors and slow their growth.
Hormone therapy is often effective initially, but some cancers may become resistant over time. This condition is known as hormone-refractory prostate cancer. Ongoing research explores new approaches to overcome resistance and improve long-term efficacy.
Managing Side Effects and Maintaining Quality of Life
Hormone therapy for prostate cancer can cause various side effects that impact a patient’s well-being. Effective management strategies and lifestyle adjustments can help alleviate these effects and improve overall quality of life.
Physical and Emotional Impacts
Hormone therapy side effects can be significant and wide-ranging. Common physical impacts include hot flashes, erectile dysfunction, fatigue, and weight gain. Patients may experience a decrease in muscle mass and bone density, increasing the risk of osteoarthritis.
The main side effects of hormone therapy are:
- Loss of muscel mass
- Lowering of Libido (sex drive)
- slower metabolism (can lead to weight gain)
Hormonal changes can lead to gynecomastia, the enlargement of breast tissue in men. Metabolic effects may raise the risk of diabetes and heart disease. Anemia is another potential concern, contributing to fatigue.
Emotionally, patients may face depression, mood swings, and cognitive changes affecting mental sharpness. These impacts can significantly alter a patient’s self-image and relationships.
Strategies for Side Effect Management
Proactive management can help mitigate many side effects. For hot flashes, patients can try cooling techniques or medications. Erectile dysfunction may be addressed with various treatments, including medications or devices.
To combat fatigue, a balanced exercise regimen is crucial. Weight-bearing exercises can help maintain muscle mass and bone density. Monitoring and managing cholesterol levels through diet and medication can reduce cardiovascular risks.
Regular check-ups and blood tests are essential to monitor for anemia, diabetes, and other metabolic changes. Medications or supplements may be prescribed to address specific issues like bone loss or anemia.
Supportive Therapies and Lifestyle Changes
Supportive therapies can play a crucial role in managing side effects. Cognitive behavioral therapy may help with depression and mood changes. Nutritional counseling can guide patients in maintaining a healthy weight and managing diabetes risk.
A balanced diet rich in fruits, vegetables, and lean proteins supports overall health. Limiting alcohol and quitting smoking can improve treatment outcomes and quality of life.
Regular exercise, including both aerobic and strength training, is vital. It helps manage weight, maintain muscle mass, and boost energy levels. Mindfulness practices or meditation can aid in stress reduction and emotional well-being.
Joining support groups allows patients to share experiences and coping strategies with others facing similar challenges.
Frequently Asked Questions
Hormone therapy for prostate cancer raises several important questions for patients and their families. Understanding the side effects, duration, timing, and effectiveness of this treatment is crucial for informed decision-making.
What are the common side effects associated with hormone therapy for prostate cancer?
Hormone therapy for prostate cancer can cause various side effects. Common issues include hot flashes, decreased libido, and erectile dysfunction. Some men experience fatigue, weight gain, and loss of muscle mass.
Mood changes and depression may occur in certain patients. Bone loss and increased risk of fractures are potential long-term side effects that require monitoring.
How long is hormone therapy typically prescribed for men with prostate cancer?
The duration of hormone therapy varies depending on the stage and aggressiveness of the cancer. For some men, it may be prescribed for a few months in conjunction with radiation therapy.
In cases of advanced prostate cancer, hormone therapy might be recommended indefinitely. Intermittent hormone therapy, alternating periods of treatment and breaks, is sometimes used to reduce side effects.
At what stage of prostate cancer is hormone therapy considered necessary?
Hormone therapy is often used for prostate cancer that has spread beyond the prostate gland. It’s also recommended for high-risk localized prostate cancer in combination with radiation therapy.
Some men with intermediate-risk prostate cancer may receive short-term hormone therapy with radiation. In early-stage, low-risk prostate cancer, hormone therapy is typically not the first-line treatment.
Can a patient opt out of hormone therapy for prostate cancer, and what are the implications?
Patients have the right to refuse any treatment, including hormone therapy. However, opting out may lead to faster cancer progression, especially in advanced cases.
For some early-stage cancers, alternative treatments like surgery or radiation might be options. Patients should discuss the potential risks and benefits of forgoing hormone therapy with their oncologist.
What is the effectiveness of combining radiation with hormone therapy in treating prostate cancer?
Combining radiation with hormone therapy has shown improved outcomes for certain prostate cancer patients. This approach can increase the effectiveness of radiation treatment.
Studies indicate that the combination therapy may reduce the risk of cancer recurrence and improve survival rates in intermediate and high-risk prostate cancers. The duration of hormone therapy alongside radiation varies based on individual risk factors.
How does the cost of hormone therapy for prostate cancer patients vary?
The cost of hormone therapy for prostate cancer can vary significantly. Factors affecting price include the type of medication, frequency of administration, and duration of treatment.
Insurance coverage plays a crucial role in out-of-pocket expenses. Some hormone therapies are available as less expensive generic versions, while others, particularly newer medications, may be more costly.