Understanding the Connection and Treatment Options for Lower Urinary Tract Symptoms.
Lower urinary tract symptoms (LUTS) affect many men as they age, often causing discomfort and impacting quality of life. These symptoms can include frequent urination, weak urine flow, and difficulty emptying the bladder completely. While LUTS can have various causes, they are frequently associated with prostate issues.
The prostate gland plays a crucial role in male urinary function, and its enlargement can lead to lower urinary tract symptoms.
As men grow older, the prostate may increase in size, potentially causing urinary problems.
This condition, known as benign prostatic hyperplasia (BPH), is common but not necessarily indicative of prostate cancer.
Understanding the connection between LUTS and prostate health is essential for proper diagnosis and treatment.
Men experiencing persistent urinary symptoms should consult a healthcare provider for a thorough evaluation, which may include physical examinations and symptom assessments.
Early intervention can help manage symptoms effectively and improve overall well-being.
Key Takeaways
- LUTS often stem from prostate enlargement and can significantly affect men’s quality of life
- Proper diagnosis involves comprehensive evaluations, including physical exams and symptom assessments
- Early consultation with healthcare providers is crucial for effective management of LUTS
Understanding Lower Urinary Tract Symptoms (LUTS) and Prostate Health
Lower urinary tract symptoms (LUTS) are closely linked to prostate health in men. These symptoms can significantly impact quality of life and may indicate underlying prostate issues.
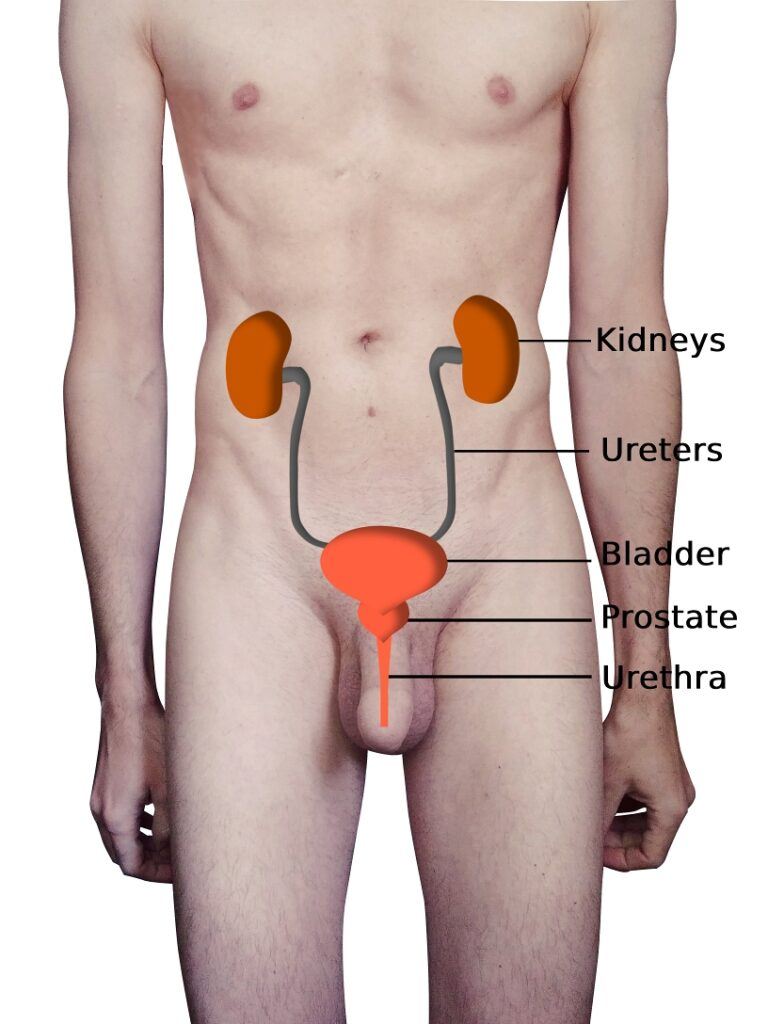
Anatomy and Physiology of the Prostate
The prostate is a walnut-sized gland located below the bladder. It surrounds the urethra and produces fluid that nourishes and protects sperm. As men age, the prostate often enlarges, which can affect urinary function.
The prostate contains smooth muscle and glandular tissue. Its size and function are regulated by hormones, primarily testosterone. Normal prostate growth occurs during puberty and early adulthood.
Benign prostatic hyperplasia (BPH) is a common condition where the prostate enlarges, potentially compressing the urethra and causing urinary symptoms.
Overview of Lower Urinary Tract Symptoms
LUTS encompass a range of urinary issues affecting the bladder, prostate, and urethra. They are categorized into three groups:
- Storage symptoms:
- Frequent urination
- Urgency
- Nocturia (nighttime urination)
- Voiding symptoms:
- Weak stream
- Straining
- Intermittent flow
- Post-micturition symptoms:
- Incomplete emptying
- Post-void dribbling
These symptoms can vary in severity and impact daily life. Men experiencing LUTS should consult a healthcare professional for proper evaluation and treatment.
Common Causes of LUTS
Multiple factors can contribute to LUTS in men. BPH is a leading cause, but it’s not the only one. Other potential causes include:
- Prostatitis (inflammation of the prostate)
- Urinary tract infections
- Bladder stones
- Neurological disorders
- Diabetes
- Metabolic syndrome
Lifestyle factors such as fluid intake, alcohol consumption, and certain medications can also influence LUTS. Age-related changes in bladder function and prostate size often play a significant role.
Proper diagnosis is crucial, as some LUTS may indicate prostate cancer. Urinary retention, frequency, and nocturia have been found to be predictive of prostate cancer in some cases.
Diagnosis and Management of Prostate-Related LUTS
Proper diagnosis and management of lower urinary tract symptoms (LUTS) related to prostate issues involve thorough clinical assessment, specific diagnostic tools, and a range of treatment approaches. Effective care also includes lifestyle modifications and supportive measures to improve patient outcomes.
Clinical Assessment of LUTS
Clinical assessment begins with a detailed patient history and physical examination. The International Prostate Symptom Score (IPSS) is a valuable tool for classifying LUTS severity and assessing quality of life impact. A digital rectal examination (DRE) is essential to evaluate the prostate’s size, consistency, and symmetry.
Urinary symptoms are carefully documented, including frequency, urgency, and nocturia. Physicians also inquire about urinary flow strength, incomplete emptying sensations, and post-micturition dribble.
A urinary frequency volume chart helps quantify fluid intake and output patterns. This chart provides insights into the patient’s voiding habits and potential contributing factors to LUTS.
Diagnostic Tools
Several diagnostic tools aid in the accurate assessment of prostate-related LUTS. The urine dipstick test is recommended to screen for infections or hematuria. Urinary flow rate measurement objectively evaluates the strength of urine flow and can indicate obstruction.
The prostate-specific antigen (PSA) test may be considered, especially in men over 50 or those with risk factors for prostate cancer. However, its use should be discussed carefully with patients due to potential overdiagnosis concerns.
In some cases, additional imaging studies like ultrasound or urodynamic testing may be necessary to assess prostate size, bladder function, or rule out other urological conditions.
Treatment Approaches for LUTS
Treatment for prostate-related LUTS is tailored to symptom severity and impact on quality of life. Alpha-blockers are often the first-line medication, helping to relax prostate and bladder neck muscles to improve urine flow.
For men with enlarged prostates, 5-alpha reductase inhibitors (5-ARIs) may be prescribed to shrink the gland over time. Combination therapy with alpha-blockers and 5-ARIs can be effective for some patients.
In cases of severe symptoms or medication-resistant LUTS, surgical interventions may be considered. These include:
- Transurethral resection of the prostate (TURP)
- Transurethral incision of the prostate (TUIP)
- Holmium laser enucleation of the prostate (HoLEP)
Each procedure has specific indications and potential benefits based on prostate size and patient factors.
Lifestyle Management and Supportive Care
Lifestyle modifications play a crucial role in managing prostate-related LUTS. Patients are advised to limit fluid intake before bedtime to reduce nocturia. Avoiding bladder irritants like caffeine and alcohol can help improve symptoms.
Pelvic floor exercises may be recommended to enhance bladder control. Double voiding techniques can assist in more complete bladder emptying.
For overweight patients, weight loss is encouraged as it can reduce pressure on the bladder and improve LUTS. Regular physical activity also shows benefits in symptom management.
Supportive care includes patient education about the natural course of LUTS and realistic treatment expectations. Regular follow-ups ensure timely adjustments to the management plan as needed.
Frequently Asked Questions
Lower urinary tract symptoms (LUTS) can affect both men and women, with various causes and treatment options. Understanding the symptoms, differences between genders, and available therapies is crucial for effective management.
What are common symptoms indicating Lower Urinary Tract Symptoms (LUTS) in males?
Males with LUTS often experience frequent urination, urgency, and a weak urine stream. They may also have difficulty starting urination, feel the need to urinate again shortly after emptying the bladder, and experience dribbling after urination.
These symptoms can significantly impact daily life and sleep quality. An enlarged prostate gland is a common cause of LUTS in men.
How does Lower Urinary Tract Symptoms manifest in females?
Females with LUTS may experience urgency, frequency, and incontinence. They might feel a sudden, strong urge to urinate and have difficulty holding it.
Nocturia, or the need to urinate multiple times during the night, is also common. Women may experience pain or discomfort in the lower abdomen or during urination.
What are the most effective treatments for Lower Urinary Tract Symptoms (LUTS)?
Effective treatments for LUTS include lifestyle modifications, medications, and in some cases, surgical interventions. Bladder training and pelvic floor exercises can help improve bladder control.
Alpha-blockers and 5-alpha reductase inhibitors are commonly prescribed medications for men with enlarged prostates. For overactive bladder symptoms, anticholinergics or beta-3 agonists may be recommended.
What are the latest advancements in the treatment of an enlarged prostate?
Recent advancements in treating enlarged prostates include minimally invasive procedures like Optilume BPH Turbo, UroLift and Rezum. These treatments aim to reduce prostate size and improve urine flow with fewer side effects than traditional surgery.
Newer medications targeting specific prostate receptors are also being developed. These aim to provide better symptom relief with fewer side effects.
How can one differentiate between symptoms of a urinary tract infection and an enlarged prostate?
Urinary tract infections (UTIs) often cause burning during urination, cloudy or bloody urine, and fever. These symptoms are typically not present with an enlarged prostate.
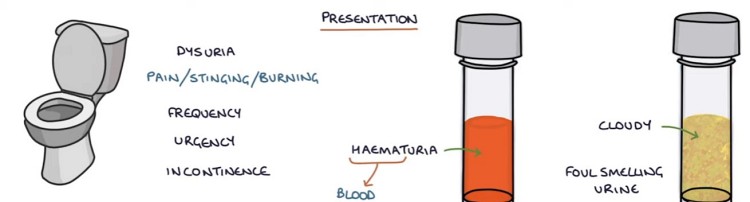
Prostate enlargement tends to cause more gradual onset of symptoms, while UTIs often develop more rapidly. A urine test can help differentiate between the two conditions.
Do prostate issues increase the risk of urinary tract infections?
Yes – Prostate issues can indeed increase the risk of urinary tract infections. An enlarged prostate can lead to incomplete bladder emptying, which creates an environment where bacteria can thrive.
Men with chronic prostatitis or benign prostatic hyperplasia (BPH) may be more susceptible to UTIs. Regular check-ups and proper management of prostate conditions can help reduce this risk.